Are Antibody-Drug Conjugates The Next Big Cancer Breakthrough?
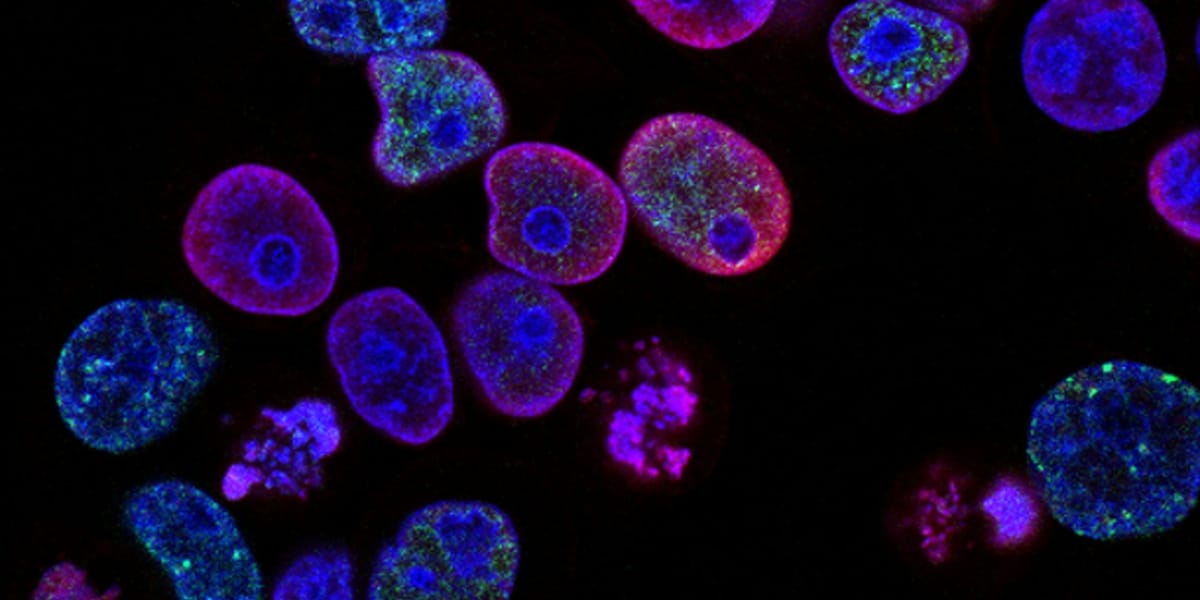
Cancer remains a significant global health challenge, with increasing incidence and mortality rates. Traditional cancer treatments, such as chemotherapy and radiotherapy, often lack specificity, leading to substantial side effects. Antibody-drug conjugates (ADCs) have emerged as a promising therapeutic approach, offering targeted delivery of cytotoxic payloads to cancer cells, thereby minimizing off-target toxicity. This review summarizes the current state of ADC development, focusing on their design, mechanisms of action, and clinical applications.
Design and Mechanism of Action
ADCs are composed of three key components:
- Antibody: A monoclonal antibody specifically recognizes and binds to a tumor-associated antigen (TAA) expressed on the surface of cancer cells.
- Linker: A chemical linker connects the antibody to the cytotoxic payload. Linkers can be cleavable or non-cleavable, influencing drug release mechanisms.
- Payload: A potent cytotoxic agent, such as a chemotherapeutic drug or a toxin, is responsible for killing the targeted cancer cells.
The mechanism of action of ADCs involves several steps:
- Target Binding: The antibody component of the ADC binds to the TAA on the cancer cell surface.
- Internalization: The ADC-TAA complex is internalized into the cancer cell through receptor-mediated endocytosis.
- Payload Release: The linker is cleaved within the cell, releasing the cytotoxic payload.
- Cell Death: The payload exerts its cytotoxic effect, leading to cancer cell death.
Clinical Applications
Several ADCs have received regulatory approval for the treatment of various cancers, including:
- Brentuximab vedotin (Adcetris): Approved for Hodgkin lymphoma and systemic anaplastic large cell lymphoma.
- Trastuzumab emtansine (Kadcyla): Approved for HER2-positive metastatic breast cancer.
- Inotuzumab ozogamicin (Besponsa): Approved for CD22-positive B-cell precursor acute lymphoblastic leukemia.
Many other ADCs are in clinical trials, targeting a wide range of cancers.
Advancements and Challenges
Recent advancements in ADC development include:
- Site-specific conjugation: Improved conjugation techniques enable precise attachment of the payload to specific sites on the antibody, enhancing stability and efficacy.
- Novel payloads: Development of new cytotoxic agents with enhanced potency and reduced toxicity.
- Bispecific antibodies: These antibodies can bind to two different targets, increasing the range of targetable cancers.
However, challenges remain in ADC development, including:
- Drug resistance: Cancer cells can develop resistance to ADCs through various mechanisms, such as reduced TAA expression or altered intracellular trafficking.
- Adverse effects: ADCs can cause side effects, such as hepatotoxicity and neutropenia.
- Tumor heterogeneity: Tumors are composed of diverse cell populations, some of which may not express the target antigen, limiting ADC efficacy.
Future Directions
Future research in ADC development is focused on overcoming the aforementioned challenges. Strategies include:
- Identifying novel TAAs: Expanding the range of targetable cancers by identifying new TAAs that are highly expressed on cancer cells and minimally expressed on normal cells.
- Developing more potent and less toxic payloads: Identifying new cytotoxic agents with improved therapeutic index.
- Combining ADCs with other therapies: Enhancing efficacy by combining ADCs with other cancer treatments, such as immunotherapy or chemotherapy.
Conclusion
ADCs represent a significant breakthrough in cancer therapy, offering targeted delivery of cytotoxic payloads to cancer cells. While challenges remain, ongoing research and development efforts are expected to further improve the efficacy and safety of ADCs, expanding their clinical applications and benefiting a wider range of cancer patients.
References
- Parit, S., et al. (2024). Antibody-Drug Conjugates: A promising breakthrough in cancer therapy. International Journal of Pharmaceutics, 124211.
- Knox, 2010
- Quinteros et al., 2017
- Tsuchikama and An, 2018
- Chehelgerdi et al., 2023, Alley et al., 2010
- Demlie et al., 2020
- Huang et al., 2020
- Hamilton, 2015
- Staben et al., 2016
- Peters and Brown, 2015
- Lambert and Morris, 2017
- Lambert and Berkenblit, 2018
- Agarwal and Bertozzi, 2015
- Birrer et al., 2019
- Al Meslamani and Bostanudin, 2023
- Chudasama et al., 2016
- Rao et al., 2015
- Gong et al., 2018
- Duerr and Friess, 2019
- Dokter et al., 2014, Dean-Colomb and Esteva, 2008
- Walko and H. (Jack), 2019
- Golfier et al., 2014, Staudacher and Brown, 2017, Najminejad et al., 2023
- Singh et al., 2016



